THE MPOX MENACE: A TICKING TIME BOMB BY DIM CHINWENDU ASSUMPTER
UNTHNEWSONLINE
Edited by Uchelue Boniface and Okoruwa Patrick.
Recently, the world has been shocked with the surge of the monkey pox diseases across the globe. Unfortunately, many people do not know the weight of these developing catastrophes that will befall the human race, if appropriate measures are not put in place to address this viral disease. This report is my little contribution to help people understand the reality of Mpox infection and how to stay safe from it. Enjoy the write-up.
Mpox, also known as Monkey pox, is a viral illness caused by the Monkey pox virus (MPXV). It is an enveloped double-stranded DNA virus of the Orthopox virus genus in the Pox viridae family, which includes Variola, cowpox, Vaccinia, and other viruses.
According to World Health Organization, in August 2024, there are two distinct clades of the virus: Clade I (with sub clades 1a and 1b) and clade II(with sub clades 11a and 11b).
In 2022-2023, a global outbreak of Mpox was caused by the clade 11b strain. Mpox continues to be a threat today as an upsurge of cases in the Democratic Republic of Congo and other countries caused by clade 1a and 1b has raised concern.
SYMPTOMS OF MPOX:
According to World Health Organization, August 2024, symptoms of mpox include:
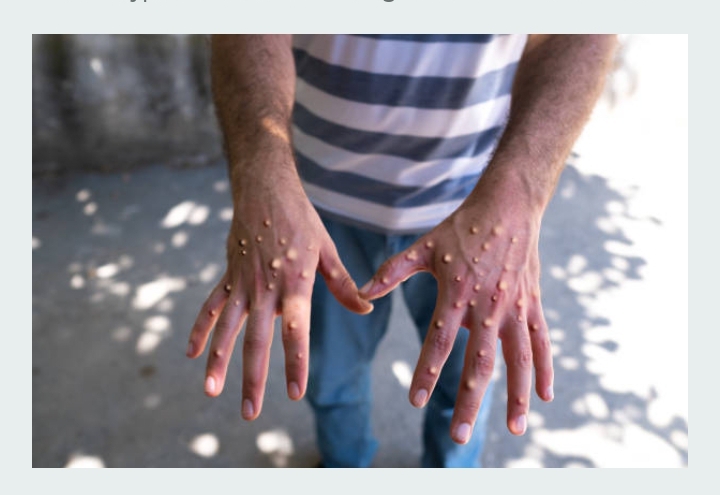
Skin rash – which can last 2-4 weeks, accompanied by fever, headache, muscle aches, back pain, low energy and swollen lymph nodes.
A publication from Center for Disease Control (cdc.gov) on clinical features of Mpox stated several modes through which Mpox can be transmitted, which include:
1. Close contact with infected individuals:
*Direct skin-to-skin contact – This involves touching the rash, scabs, or body fluids of a person with Mpox. *Intimate contact – activities such as hugging, kissing, and sexual contact can spread the virus. *Respiratory secretions – prolonged face-to-face contact or close-range interactions can transmit the virus through respiratory droplets from talking, sneezing, or coughing.
2. Contact with contaminated objects:
*Fomites – the virus can survive on surfaces and objects like clothing, bedding, towels, and other personal items that have been used by an infected person.
3. Animal to Human Transmission:
*Infected Animals—Mpox can spread from animals to humans through bites, scratches, or direct contact with the animal’s body fluids or lesions.
*Consumption of infected animals: Handling or consuming meat from infected animals can also be a source of transmission.
4. Vertical Transmission;
*Pregnancy and Birth- An infected pregnant woman can pass the virus to the fetus during pregnancy or to the newborn during and after birth.
According to a publication from Center for Disease Control and Prevention, a United States Federal Agency, September 2024. Mpox undergoes these stages of development:
Incubation Period –
*This period lasts about 1-2 weeks after infection.
*At this stage, symptoms are not visible and are not contagious
2. Prodrome –
*Early symptoms appear, including fever, headache, muscle aches, back pain, swollen lymph nodes and fatigue.
*Swollen lymph_ nodes is a distinguishing feature_of Mpox, at this stage, it is contagious.
3. Rash –
The rash starts within 1-3 days after the onset of fever.
It passes through these stages:
a) Macules: The rash is flat, discolored lesions.
b) Papules: it changes to raised lesions.
c) Vesicles: lesions filled with clear fluid.
d) Pustules: lesions filled with yellowish fluid which eventually dip at the centre, giving an umbilicated appearance.
e) Scabs: The rash becomes hard, crusty patches that eventually fall off as the lesions heal.
f) Resolution: The lesions scab over and fall off, leaving the skin healed.
BRIEF HISTORY OF MONKEY POX IN NIGERIA
As stated by the World Health Organization, (WHO) and National Centre for Biotechnology Information, (NCBI), Monkey Pox was first detected on April 4, 1971.
A 4-year-old girl living in Ihie-Imuduru village in Abia State, South-East Nigeria, developed a febrile illness associated with generalized vesiculopustular skin lesions. Nine days later, her 24 year-old mother also developed fever and skin rash. Following laboratory investigation, the child was confirmed, as the first human case of Monkey pox in Nigeria.
After that incident, in September 2017, there was a suspected outbreak of Monkey pox in Yenagoa, Bayelsa State. The index cluster was reported in a family. All of whom developed similar symptoms of fever and generalized skin rash. An epidemiological investigation showed all infected cases had contact with a monkey.
In 2018, a total of 76 cases were reported and 37 confirmed. These cases were reported in 14 states, which include Abia, Edo, Enugu, Imo, Lagos, Nasarawa, Oyo, Plateau, Rivers, and the Federal Capital Territory (FCT).
THE UNTH PERSPECTIVE
In a bid to know the efforts the UNTH is putting in place to tame this upcoming monster, I spoke with Dr. Uche Unigwe, an infectious Disease Physician and Head of the Infectious Disease Centre, University of Nigeria Teaching Hospital, Ituku/Ozalla, Enugu. He noted that Mpox is a viral zoonotic disease, which implies it is not gotten from monkeys alone but from animals in general. According to him, in Nigeria, between 2017 and 2024, there have been 4000 suspected cases, 1,134 confirmed, and 17 deaths.
Speaking further, he noted that the most vulnerable groups include the following:
Pregnant women,
Children,
Persons with HIV,
Persons with uncontrolled diabetes and
Cancer therapy patients.
He went further to state that in the Democratic Republic of Congo, where the latest epidemic is more established, there is the Clade 1b strain, which is more transmissible and suspected to cause more mortality. Dr. Unigwe noted that one thing about viruses is the potential to mutate, that is, change some of their genetic properties, thereby acquiring new characteristics. The new characteristics may make the virus milder or more transmissible and virulent.
Therefore, strict measures must be put in place.
Dr. Unigwe went on to enumerate some of the global measures which may also be used in UNTH to combat the disease. These strategic measures include;
✓ Effective sensitization of the populace about the existence of Mpox disease using various media channels.
✓ Serious surveillance should be observed at the entry points e.g.. Airports, borders, etc.
✓ There should be a form to fill to ascertain who has rash, sore throat, itching, etc.
✓ Qualified and trained health personnel should be employed to operate the infrared thermometer for correct temperature check at the entry points.
✓ Exposure to animals should be to the lowest minimum.
✓ Hand washing and constant use of alcohol- based hand sanitizers should be practiced.
✓ There should be a lot of community engagements of groups that permit sessions of one-on-one interactions. These will be most useful in educating and convincing the people about the benefit of taking vaccines.
✓ Whenever the disease is confirmed in a patient, there should be proper contact tracing so as to limit spread.
✓ There should be prompt referral and people should not hide when it is noticed.
✓ Health care workers should be educated on how to handle people with the disease so that they will not feel stigmatized
✓ Research should be carried out at the molecular level to unravel other facts about Mpox virus.
✓ Research should be carried out to identify the drugs that are most effective for the treatment of Mpox.
Dr Unigwe advised people on the behavioural factors to observe, especially at the peak of the mpox epidemic.
These include:
• Avoidance of hugging.
• Avoidance of hand shaking.
• People should stay away from the consumption of bush meat.
Also to wear long-sleeve clothing often.
Mrs. Dim is a staff of Public Relations Unit at the University of Nigeria Teaching Hospital, Ituku/Ozalla, Enugu and wishes to thank Dr. Unigwe for his invaluable contributions to this article.
Related Posts
Leave a Reply Cancel reply
Our Lastest Posts
- CMD UNTH COMMISSIONS A NURSING LAB IN THE COLLEGE
- LATE DR EGBUE HONOURED WITH A FLAG-STOP IN UNTH
- Management of Snake Bite At Home
- THE COMMONWEALTH PARTNERSHIP FOR ANTIMICROBIAL STEWARDSHIP PROJECTS IN UNTH PRESENT REPORT TO MANAGEMENT.
- QUANTUS MEDICAL FOUNDATION CONDUCTS A “CHANGE THE MANAGEMENT TRAINING” IN UNTH